7 Intraoperative Tests with a Focus on Lateral Thrust test for reducing risk of dislocations after a Reverse Shoulder Replacement Surgery.
The following tests are useful for testing stability of Reverse shoulder replacement during surgery.
- Lateral Thrust Test
- Bed Shuffle Test
- Anterior instability Test
- Posterior instability Test
- Conjoint tendon tension
- Limb Traction
- Deltoid tension
The Lateral Thrust Test, is the single most useful test in my practice, although I recommend using a cluster of tests in each case
The risk of instability is more common when RSA is performed for trauma, trauma sequelae and revision surgery. One would also see such a problem more commonly in case of complex elective primary shoulder replacements. The history of reducing instability-related complications following RSA is aligned to the history of evolution of RSA design! To understand this we would use the simple concepts of resolution of force vectors into their horizontal and vertical components (Let’s take you back to high school physics). The Grammont Style RSA was linked with distalization of the humeral component with respect to the Glenosphere. Here the effective vector of the Deltoid [F(Deltoid_net)] was in a relatively vertical position (Figure A). (Additionally, such medialisation of the center of rotation in the RSA was quite often associated with notching, and I am conscious these are linked matters. However, as I am focusing on the instability in this article, I would not delve into the notching issue here).
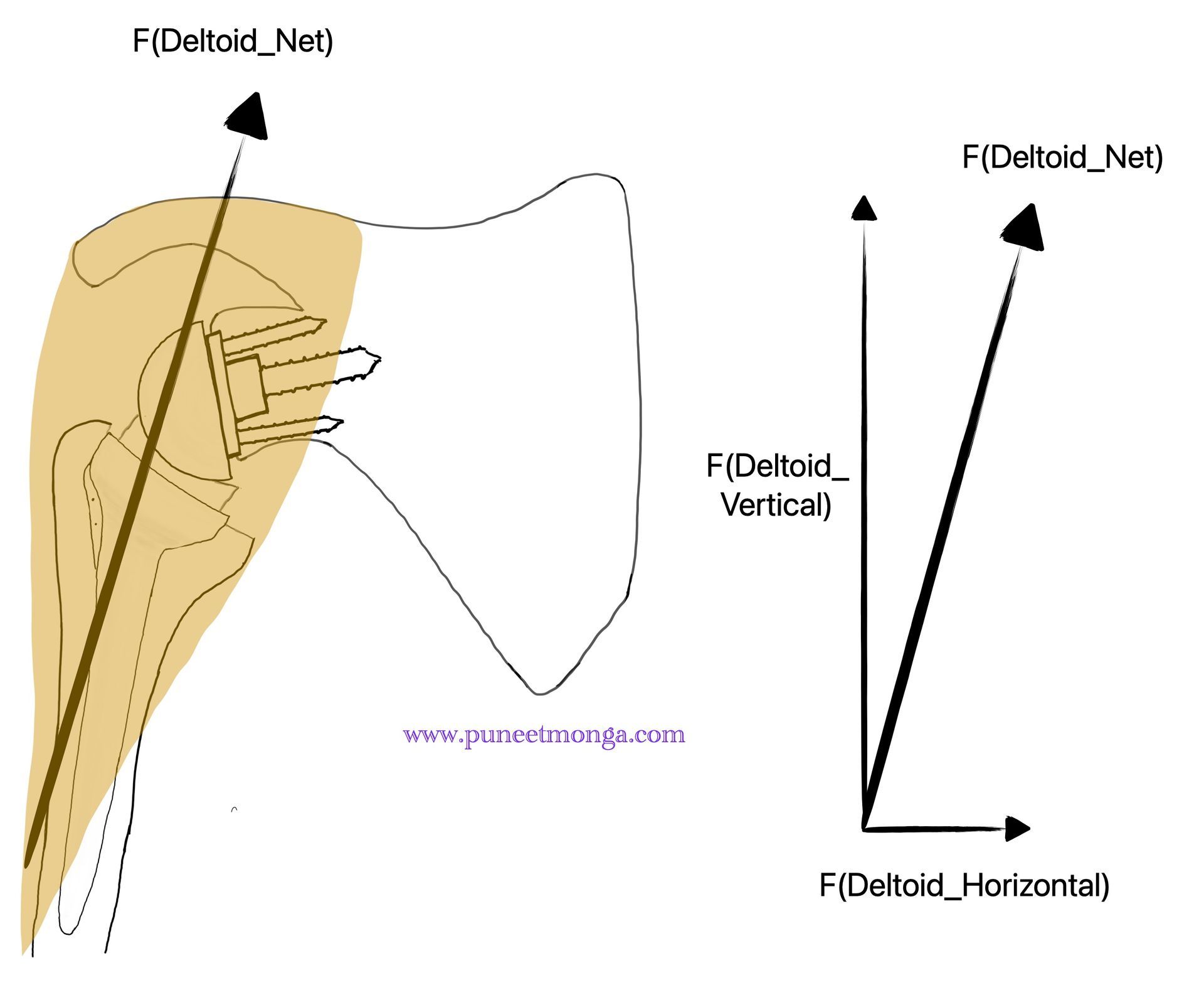
The work pioneered by Prof. Boileau, from Nice, has described how increasing the offset of the glenoid base plate would lead to improved stability of the RSA. This stability is primarily achieved by increasing the Deltoid wrap.This fascinating optimisation of joint Biomechanics relies on changing the effective force of the deltoid. Figure B demonstrates how the increasing offset at the glenoid base plate level, leads to such an alteration on the deltoid vector in the frontal plane. In this diagram, we are keeping the neck shaft angle at 155 degrees, as was described in the original Grammont style prosthesis and with the additional lateral offset at the glenoid level, we have now achieved a increased medial Deltoid vector [F(Deltoid_Horizontal)].
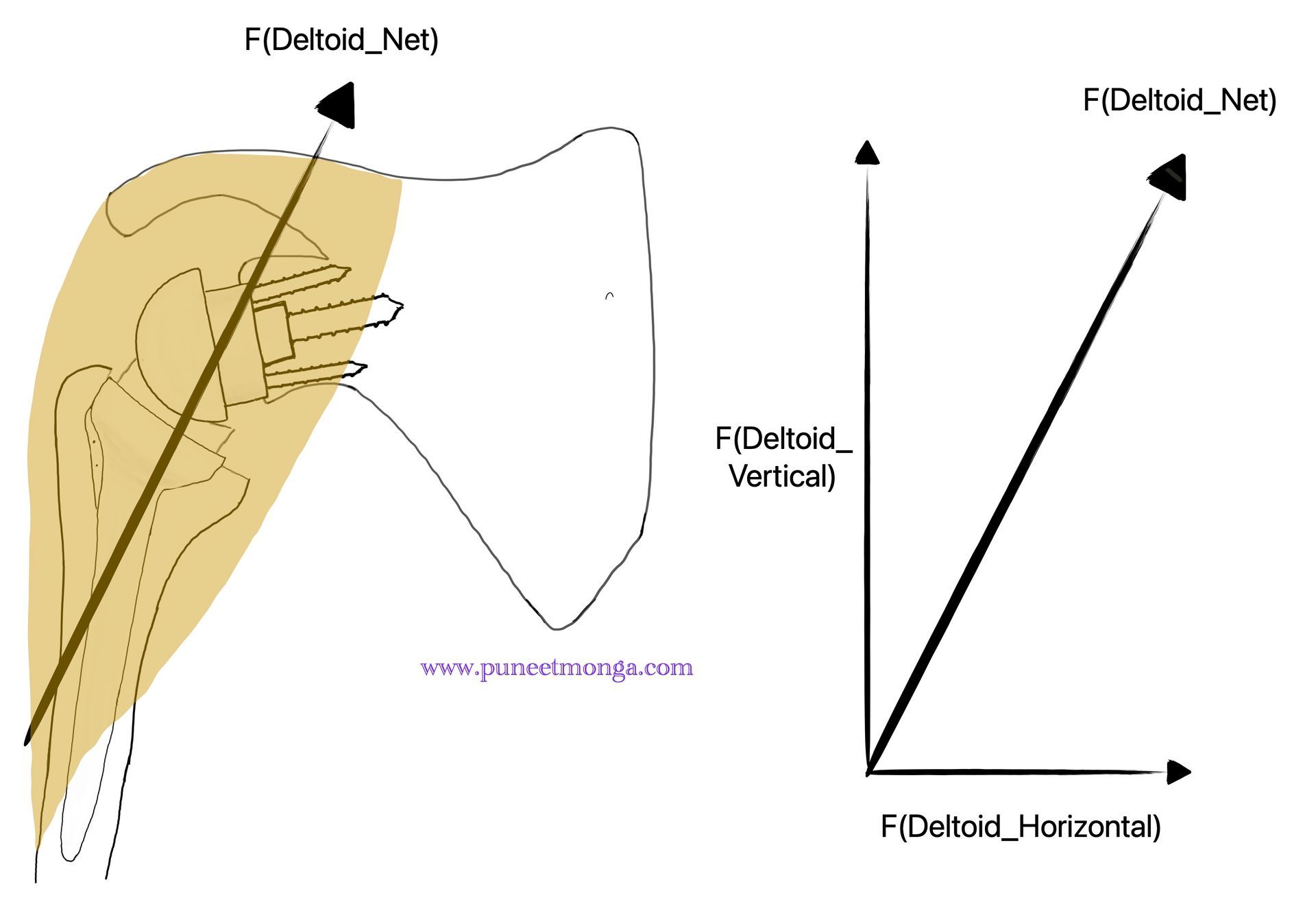
The more recent design changes on the humeral stem have allowed the neck shaft angle to be placed at a 135 degrees, which further laterlises the humerus relative to the glenoid. This design change further increases the medial component of the Deltoid vector (Figure C). An increase in the medial component of the Deltoid vector leads to increased compression Force provided by the Deltoid [F(Deltoid_Horizontal)] and hence increased stability of the construct.
The relative compressive (medial) component of the Deltoid force has been increasing from position described in Figure A, through to Figure B to further increase in Figure C. In other words, we are achieving an improved Deltoid wrap.
At the time when I started performing RSA, the standard tests for assessing stability following RSA was to pull the arm distally (limb traction) to look for Gap formation between the glenosphere and the humeral component, assess anterior deltoid tension and assess conjoint tendon tension. This would, of course, be a logical testing technique when one is performing the reverse with the principles of distalising the humerus, in line with the Grammont philosophy. However, even in a case of perfectly performed and tested RSA, one would occasionally encounter postoperative dislocation! I could often hear surgeons who were referring cases into our Institute with the exasperated expression “I tested everything and it was stable during surgery!” In fact, often the surgeon would have performed the first revision after such a dislocation and increase the liner height. As this would have a minor inflenuce on the Deltoid wrap, the results of such a revision were unreliable and hence instability would occasionally recur. I remember the occasion when I personally experienced this frustrating situation in a patient I had revised for instabilty. At the time of revision, I spent a fair amount of time trialing various components and trying various tests for assessing instability during surgery. I had recently returned from having visited Prof. Boileau in Nice and was trying to get my head around how he had managed to reduce the episodes of instability dramatically by increasing glenoid offset. The thoughts around the Deltoid wrap had not completely matured at the time (in my mind at least...this was 2012!). Most certainly I could see the humeral component escaping laterally under the glenosphere as I pushed the humerus in the lateral direction. This was the time when I started using the lateral thrust test and by increasing the glenoid component offset, I was able to achieve stability in a more reliable fashion.
Over the next few years and over a course of performing many RSAs, I routinely started testing the stability using a multitude of intraoperative tests, which in my opinion were more objective then those that existed at the time. I had previously noticed that the conjoint tendon tension could be altered by flexing and extending the shoulder making the conjoint tendon lax or taut respectively. I also noticed that traction assessment of the humerus for gap formation was very dependent on the type of anesthesia and was operator dependent. So was the deltoid tension assessment. We came up with four tests for assessing intraoperative stability following RSA including the lateral thrust test, the bed shuffle test, the anterior instability and the posterior instability tests. This work was published in 2019. Of these tests, I have found that the lateral thrust test has been the single most important test over the years. Having performed hundreds of RSAs since the routine use of these tests, we have noticed a dramatic reduction in instability following RSA.
The intraoperatively performed lateral thrust test essentially involves placing the surgeons’ finger or a bone lever medial to the humeral metaphysis and pushing laterally. One is looking for opening of the space between the humeral and glenoid components. Upto 5 to 7mm of lateral play would be considered acceptable. Importantly, there is some variation of what one would be able to achieve in terms of this lateral play, depending on the implant design. For example, when using the Ascend Flex component which has a raised medial lip of the humeral liner, one would get more a millimeter or two of lateral play. On the other hand when using a Perform stem with a symmetric liner or a symmetric liner of a Lima SMR stem (which I use with customized joint replacement), 5 to 7 millimeters of lateral thrust movement would expected. What is crucial is that the articulation should not dislocate easily on application of the lateral thrust.
What is interesting is that the amount of force that one may apply can be variable. Over the course of having trained many fellows this variability is obvious. Suffice to say, one needs to use moderate force with the humerus aligned to the trunk and in neutral rotation The variability in the amount of force may be taught during the mentoring process although further work related to quantifying this would be valuable.
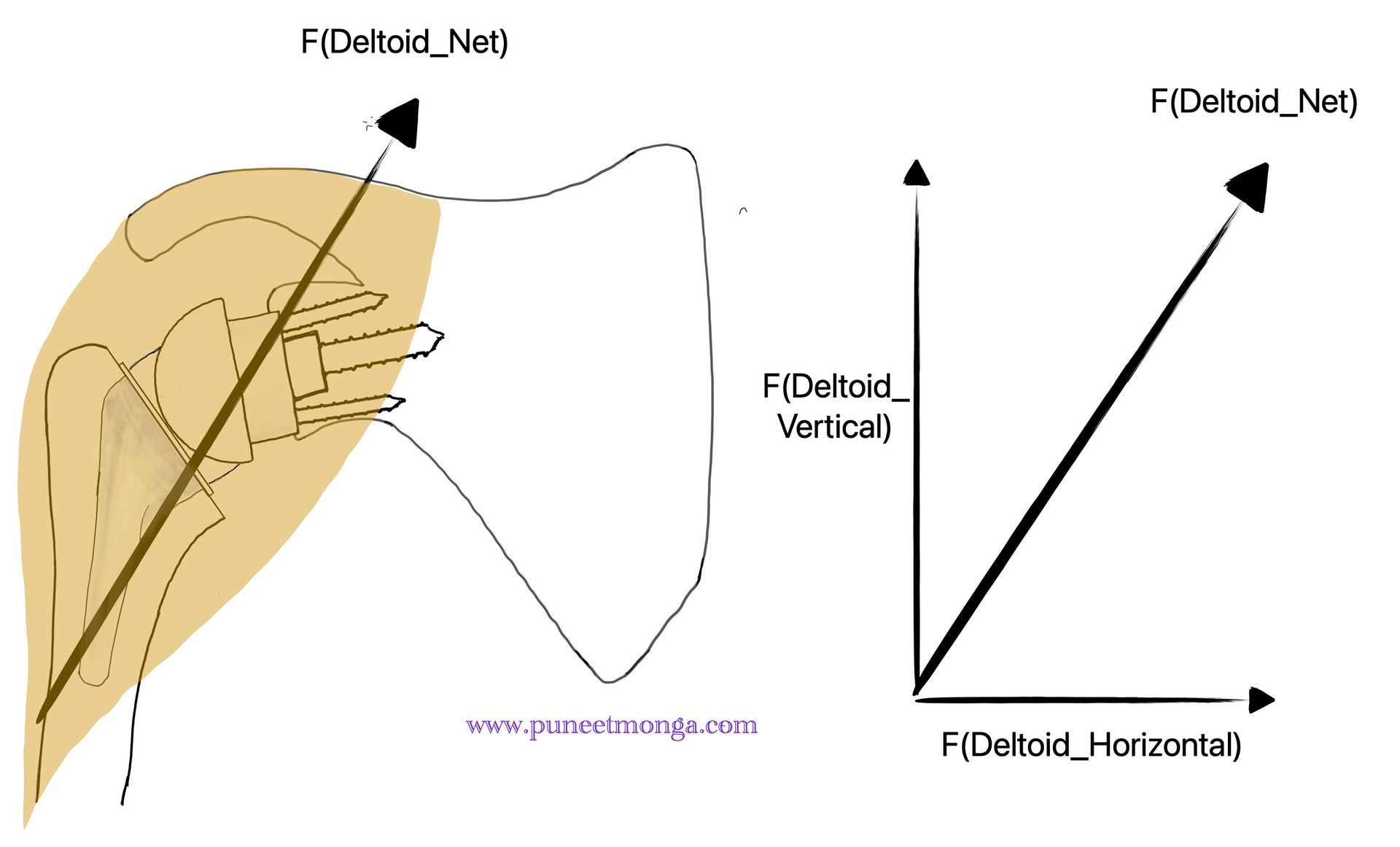
The essential principle of the lateral thrust test is the ability to check for restoration of the medial component of the deltoid wrap. If the lateral force applied during the test is proportional to the medial component of the deltoid wrap achieved by the RSA configuration, we would have stability (Figure D)

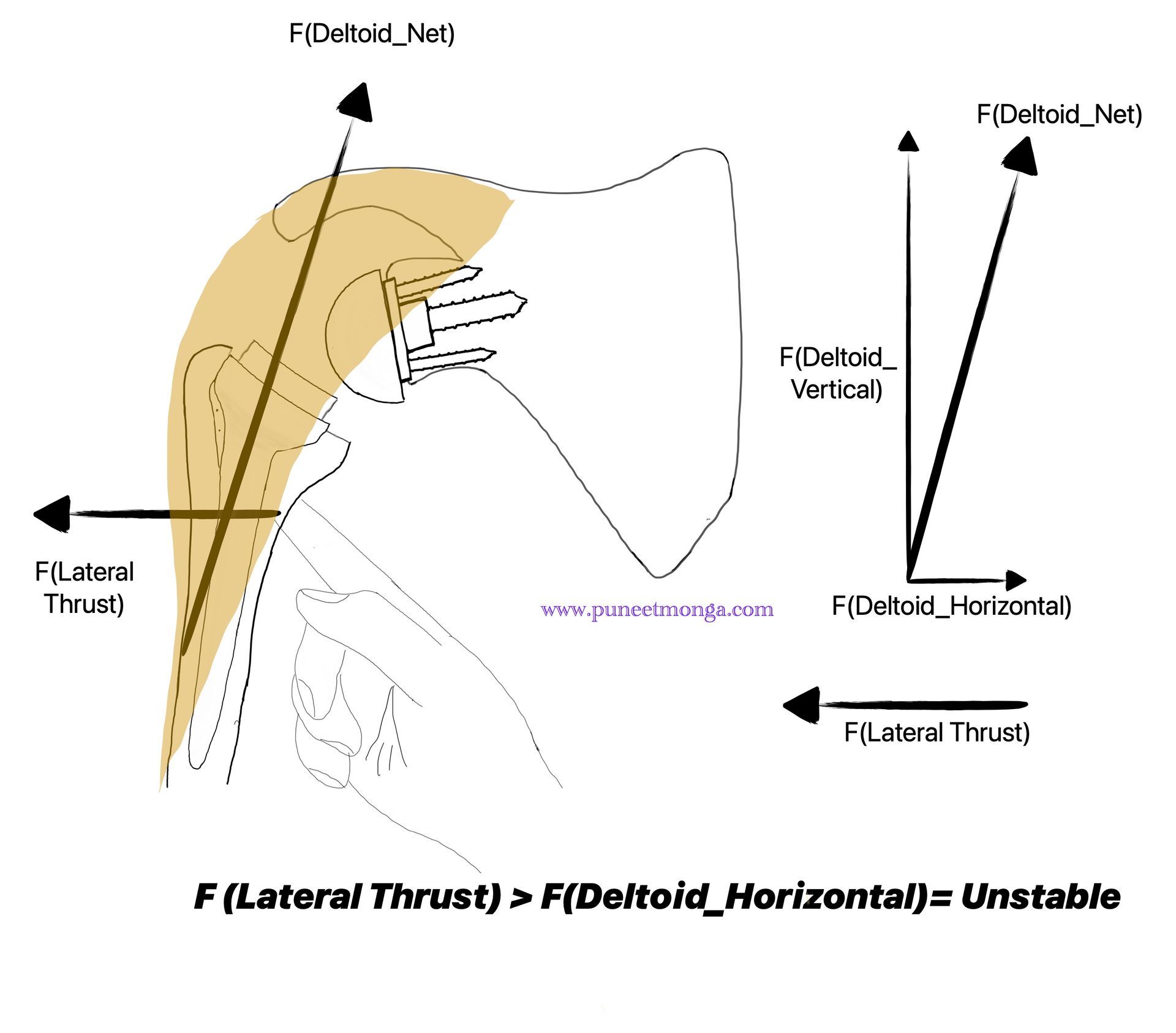
In case this lateral force is more than the forces achieved with the deltoid wrap, we are facing potential post operative instability (Figure E)
It has been my personal experience that using the lateral thrust test has significantly reduced the episodes of dislocation of RSA in my practice, with a few notable exceptions. The exception relates to soft tissue problems and my attention has been drawn to their importance in recent complex cases. I remember a case where there had been multiple surgeries related to previous deep infection. The patient had an extensively scarred deltoid and multiple attempts at restoring stability were unsuccessful, eventually leading to a suboptimal outcome of excision arthroplasty. I would recommend reading Mark Frankle and his teams’ work on instability after RSA which focuses in this category of patients as well. In the absence of a well function deltoid, the lateral thrust test would be less reliable. In other words, in the absence of optimal Deltoid wrap, we have an increased risk of instability.
The lateral thrust test, in my opinion, has been implant agnostic. With the plethora of implant choices available commercially, with a mind boggling array of designs, we need to be able to use tests which work across all designs. This is certainly valid and needed in my surgical practice. Even though I use certain implants commonly for my routine surgical practice, I am often receiving patients for revision of RSA with pre-existing well fixed implants of alternative makes. I have found the lateral thrust test to be a reliable indicator for stability across a spectrum of commercially available RSA.
This test has its own limitations. Like I mentioned, in the cases of non functional Deltoid this test is less valuable. Also, there is subjectivity related to the amount of force to be applied to achieve the lateral thrust. I am also concerned that excessive deltoid tension (too tight on lateral thrust test) would predispose to stress fractures. The science around this aspect is still evolving and I am currently unsure of an objective way of assessing excessive lateralisation during surgery. I am very conscious that a surgeon might opt to reduce the risk of dislocation in the early post operative period and trade instability for increased risk of stress injuries. Finally the interplay between optimal distalization and lateralisation needs further work. As these aspects become clearer, one will need to assess if the intraoperative assessment needs to change as well.
One can view the Lateral Thrust test as a practical tool for assessing Deltoid wrap
I hope you found this article useful and I would appreciate any feedback.
Prof. Puneet Monga is a Consultant Orthopaedic Surgeon with a special interest in shoulder problems. His works at Wrightington Hospital, which is a Specialist Orthopaedic Unit . His clinical and research work is focussed around shoulder replacements and rotator cuff problems. He can be reached on http://www.puneetmonga.com/contact
References
- Review of Orthopaedics: Expert Consult - Online and Print Paperback – 27 Mar. 2008 by Mark D Miller
(Author), Michael Carcel
(Illustrator)
- Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005 Jan-Feb;14(1 Suppl S):147S-161S. doi: 10.1016/j.jse.2004.10.006. PMID: 15726075.
- Boileau P, Morin-Salvo N, Gauci MO, Seeto BL, Chalmers PN, Holzer N, Walch G. Angled BIO-RSA (bony-increased offset-reverse shoulder arthroplasty): a solution for the management of glenoid bone loss and erosion. J Shoulder Elbow Surg. 2017 Dec;26(12):2133-2142. doi: 10.1016/j.jse.2017.05.024. Epub 2017 Jul 20. PMID: 28735842.
- Javed S, Imam MA, Monga P. Intraoperative stability assessment in reverse shoulder arthroplasty. J Clin Orthop Trauma. 2019 May-Jun;10(3):617-619. doi: 10.1016/j.jcot.2018.11.006. Epub 2018 Nov 19. PMID: 31061600; PMCID: PMC6494761.
- https://www.stryker.com/dk/en/trauma-and-extremities/products/tornier-flex/index-eu.html
- https://www.stryker.com/hk/en/trauma-and-extremities/products/tornier-perform.html
- https://limacorporate.com/en/product-detail/64/smr-reverse.html
- Melbourne C, Munassi SD, Ayala G, Christmas KN, Diaz M, Simon P, Mighell MA, Frankle MA. Revision for instability following reverse total shoulder arthroplasty: outcomes and risk factors for failure. J Shoulder Elbow Surg. 2023 Jun;32(6S):S46-S52. doi: 10.1016/j.jse.2023.01.023. Epub 2023 Feb 22. PMID: 36822501.
- Werthel JD, Walch G, Vegehan E, Deransart P, Sanchez-Sotelo J, Valenti P. Lateralization in reverse shoulder arthroplasty: a descriptive analysis of different implants in current practice. Int
- Orthop. 2019 Oct;43(10):2349-2360. doi: 10.1007/s00264-019-04365-3. Epub 2019 June 28. PMID: 31254018.
- Colasanti CA, Mercer NP, Contreras E, Simovitch RW, Zuckerman JD. Reverse shoulder arthroplasty design-inlay vs. onlay: does it really make a difference? J Shoulder Elbow Surg. 2024 Sep;33(9):2073-2085. doi: 10.1016/j.jse.2024.02.027. Epub 2024 Apr 4. PMID: 38582254.